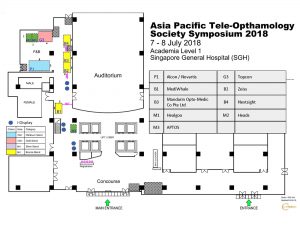
All the booths are now sold out. Potential corporate partners can consider other sponsorship opportunities. Click here for the sponsorship prospectus.
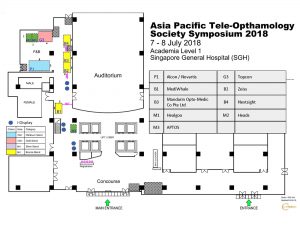
All the booths are now sold out. Potential corporate partners can consider other sponsorship opportunities. Click here for the sponsorship prospectus.